Learn about probiotic benefits and immune regulation for systemic health.
The Breath-Gut Connection: The Role of Gut Health in Pulmonary Inflammation
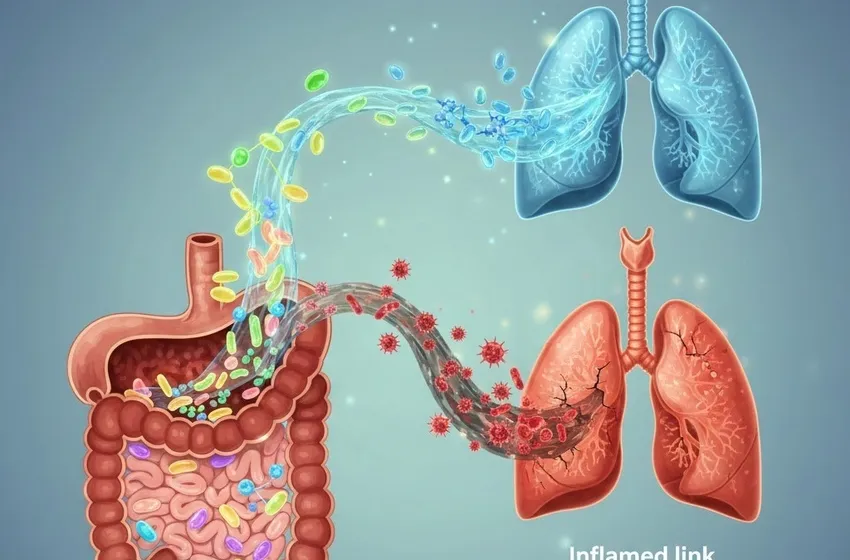
For decades, medical science treated the digestive and respiratory systems as two distinct entities. However, groundbreaking research has revealed a profound biological dialogue between these organs, known as the gut-lung axis. This bidirectional communication pathway suggests that the state of your microbiome—the trillions of microorganisms living in your intestines—plays a pivotal role in determining the severity of pulmonary inflammation and your overall susceptibility to respiratory disease.
Understanding this connection is more than just a scientific curiosity; it is a vital component of systemic health and a new frontier in preventative medicine.
What is the Gut-Lung Axis?
The gut-lung axis refers to the biochemical signaling that occurs between the gut microbiota and the lungs. While these organs are physically distant, they are linked through the lymphatic system and the bloodstream.
When the gut microbiome is balanced (homeostasis), it produces metabolites—specifically short-chain fatty acids (SCFAs) like acetate, propionate, and butyrate. These metabolites travel through the blood to the lungs, where they act as signaling molecules to keep the immune system "calm" and prevent overreactions to environmental triggers.
The Mechanism of Communication
- Metabolite Signaling: SCFAs produced in the gut bind to receptors in the lung tissue, promoting an anti-inflammatory environment.
- Immune Cell Trafficking: Immune cells "trained" in the gut can actually migrate to the lungs to help fight off pathogens.
- The Vagus Nerve: This "superhighway" of the nervous system connects the enteric nervous system to the respiratory center, allowing for rapid neurological feedback.
The Inflammation Link: How a Leaky Gut Leads to Heavy Lungs
The inflammation link between the gut and the lungs becomes evident when the intestinal barrier is compromised. This condition, often called "leaky gut," allows bacterial toxins (lipopolysaccharides or LPS) to enter the bloodstream.
Once these toxins reach the pulmonary circulation, they trigger a cascade of pro-inflammatory cytokines. This systemic "fire" can exacerbate chronic conditions such as:
- Asthma: High levels of gut dysbiosis are frequently linked to airway hyper-responsiveness.
- COPD: Chronic obstructive pulmonary disease patients often show a distinct, less diverse gut microbiome profile.
- Cystic Fibrosis: The microbiome plays a role in the frequency of pulmonary exacerbations in CF patients.
By addressing the root cause of systemic inflammation in the digestive tract, we can effectively dampen the inflammatory signals reaching the delicate tissues of the lungs.
Immune Regulation and the Microbiome
The primary job of the gut microbiome is immune regulation. Approximately 70-80% of the body’s immune cells reside in the Gut-Associated Lymphoid Tissue (GALT).
When the microbiome is diverse and healthy, it teaches the immune system to distinguish between harmless particles (like pollen or dust) and dangerous pathogens (like viruses or bacteria). If the gut is in a state of dysbiosis, the immune system becomes "jittery," leading to an overblown inflammatory response in the lungs when a minor irritant is inhaled.
Probiotic Benefits: Reinforcing the Respiratory Shield
Can we "eat" our way to better lung health? The research into probiotic benefits suggests a resounding yes. Specific strains of bacteria, such as Lactobacillus and Bifidobacterium, have been shown to:
- Enhance Mucosal Immunity: Increasing the production of secretory IgA, the first line of defense in the lungs.
- Reduce Infection Duration: Studies indicate that individuals with a healthy gut recover faster from common viral respiratory infections.
- Modulate T-cells: Shifting the immune response from a pro-inflammatory Th2 state to a more balanced Th1/Treg state.
Key Probiotic Strains for Lung Support
| Strain | Primary Benefit |
|---|---|
| L. rhamnosus GG | Reduces the risk of upper respiratory tract infections. |
| B. lactis | Enhances cellular immunity in the elderly. |
| L. plantarum | Helps modulate the systemic inflammatory response. |
Optimizing Gut Health for Systemic Health
To achieve true systemic health, we must look beyond supplements and focus on a lifestyle that supports microbial diversity. The lungs are effectively the "downstream" recipients of the gut's health status.
Dietary Strategies
- High-Fiber Intake: Fiber is the primary fuel for the bacteria that produce lung-protective SCFAs.
- Polyphenols: Found in berries, green tea, and dark chocolate, these compounds act as prebiotics.
- Fermented Foods: Natural sources of probiotics like kefir, sauerkraut, and kimchi provide live cultures to the gut.
Environmental Factors
Avoid the overuse of antibiotics when not strictly necessary, as they can "carpet bomb" the gut microbiome, leaving the lungs vulnerable to secondary infections for months afterward.
Conclusion: A New Paradigm for Pulmonary Care
The gut-lung axis represents a shift in how we approach respiratory medicine. By focusing on immune regulation via the gut, we move from merely treating symptoms of lung disease to addressing the systemic environment that allows inflammation to thrive.
Through a combination of fiber-rich diets, targeted probiotic benefits, and an understanding of the inflammation link, we can breathe easier knowing that the secret to healthy lungs may just lie in our gut.