Learn how inherited heart disease and family history impact CVD risk.
Understanding the Role of Genetics and Family History in Cardiovascular Disease (CVD)
Cardiovascular disease (CVD) remains the leading cause of mortality globally. While lifestyle choices like diet and exercise are frequently discussed, the biological blueprint we inherit plays a profound role in our heart health. Understanding the intersection of inherited heart disease, family history, and genetic testing is essential for proactive prevention and personalized care.
When Family History Becomes a Major Concern
Not all family histories of heart disease carry the same weight. While many people have an elderly relative who suffered a stroke or heart attack, clinical concern spikes when there is a pattern of early onset heart disease.
Defining "Early Onset"
Medical professionals typically identify a significant genetic risk when a primary relative (parent or sibling) experiences a major cardiac event at a young age. Specifically, a family history is a major concern if:
- A male first-degree relative (father or brother) was diagnosed before age 55.
- A female first-degree relative (mother or sister) was diagnosed before age 65.
If multiple family members are affected, or if the disease appears in consecutive generations, the likelihood of a strong genetic predisposition increases significantly.
The Spectrum of Inherited Heart Disease
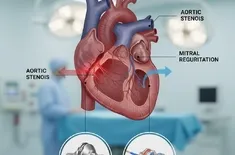
Inherited heart disease refers to conditions passed down through families via specific genetic mutations. Unlike general "heart disease," which is often a mix of lifestyle and environment, inherited conditions are often "monogenic," meaning they are caused by a mutation in a single gene.
Common Inherited Conditions
- Familial Hypercholesterolemia (FH): A genetic disorder that leads to dangerously high LDL (bad) cholesterol levels from birth, significantly increasing the risk of early heart attacks.
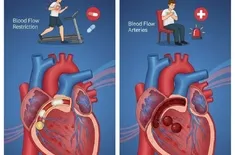
- Hypertrophic Cardiomyopathy (HCM): A condition where the heart muscle becomes abnormally thick, making it harder for the heart to pump blood.
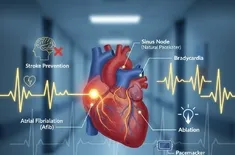
- Long QT Syndrome: A heart rhythm disorder that can cause fast, chaotic heartbeats.
The Power of Genetic Testing and Screening
Modern medicine has moved toward "precision cardiology." We no longer have to wait for symptoms to appear before taking action.
The Value of Screening
Regular screening is the first line of defense. This includes monitoring blood pressure, cholesterol panels, and blood glucose levels. For those with a known family history, these screenings should begin much earlier in life than for the general population.
Genetic Testing: A Roadmap to Prevention
Genetic testing involves analyzing DNA to identify specific mutations associated with CVD. This is particularly useful for:
- Identifying "silent" carriers within a family.
- Tailoring medication (pharmacogenomics).
- Providing peace of mind or a clear roadmap for lifestyle interventions.
Balancing Genetics with Modifiable Risk Factors
It is a common misconception that "genetics is destiny." In reality, your genetic makeup often determines your baseline risk, but your environment and choices determine whether that risk manifests as disease. These are known as modifiable risk factors.
Key Modifiable Factors
- Tobacco Use: Smoking multiplies the risk of heart disease exponentially in those already genetically predisposed.
- Dietary Habits: Diets low in saturated fats and high in fiber can help manage cholesterol levels that may be genetically elevated.
- Physical Activity: Regular exercise strengthens the heart muscle and improves vascular health.
- Weight Management: Reducing adipose tissue lowers systemic inflammation, a key driver of CVD.
Even if you have a high genetic risk score, aggressive management of these modifiable risk factors can often "override" your DNA, delaying or preventing the onset of disease.
Integrating Clinical Care and Personal Awareness
If you suspect your family has a history of heart issues, the next steps are crucial.
Step-by-Step Action Plan
- Document Your Pedigree: Talk to relatives. Find out who had heart issues and, crucially, at what age they were diagnosed.
- Consult a Genetic Counselor: These professionals can help interpret family patterns and determine if genetic testing is appropriate.
- Early Intervention: If a genetic risk is identified, start screening for cholesterol and blood pressure in your 20s or even earlier if recommended by a pediatrician.