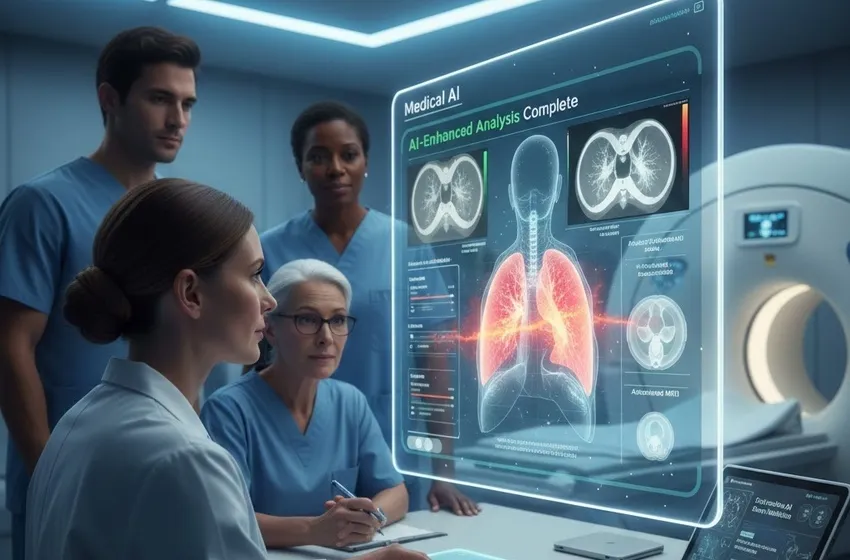
Explore how Generative AI and deep learning transform diagnostic imaging.
The Frontier of Modern Medicine: Generative AI in Diagnostic Imaging
The landscape of clinical diagnostics is undergoing a profound transformation. At the heart of this shift is Generative AI, a subset of artificial intelligence that doesn't just analyze data—it creates it. In the realm of diagnostic imaging, this technology is moving beyond simple pattern recognition to become a fundamental partner for clinicians. By leveraging deep learning architectures, particularly Generative Adversarial Networks (GANs) and Diffusion Models, medical AI is now capable of reconstructing high-resolution scans from minimal data, simulating disease progression, and even translating one imaging modality into another.
For radiology departments, the implications are life-changing. Traditional image analysis often struggles with noise in low-dose scans or the sheer volume of data produced by modern scanners. Generative AI addresses these bottlenecks, providing tools for early detection that were previously relegated to the realm of science fiction. By identifying subtle anomalies—the faint shadows of a nascent tumor or the microscopic irregularities in vascular walls—these systems act as a hyper-vigilant second pair of eyes, ensuring that no detail, however small, goes unnoticed.
Understanding the Core Technologies
The leap from traditional computer-aided detection to modern generative systems is powered by deep learning. Unlike older algorithms that relied on human-defined rules, deep learning models learn directly from vast datasets of clinical images.
- Generative Adversarial Networks (GANs): These consist of two neural networks—a generator and a discriminator—competing against each other. In radiology, GANs are used to create "virtual contrast" scans or to turn low-field MRI images into high-field quality results.
- Diffusion Models: These models excel at high-fidelity image reconstruction. By starting with random noise and gradually refining it into a coherent image based on learned anatomical priors, they produce scans with unprecedented clarity.
- Variational Autoencoders (VAEs): Often used for image analysis and segmentation, VAEs help in understanding the underlying structure of medical data, which is crucial for identifying how a lesion might look across different patient demographics.
Improving Clinical Outcomes Through Early Detection
The primary goal of medical AI in the diagnostic suite is to improve patient survival rates. Early detection is the cornerstone of effective treatment, especially in oncology and cardiology.
Identifying Subtle Anomalies
Human fatigue is a real factor in radiology. After reviewing hundreds of scans, a radiologist’s ability to spot a 2mm nodule may diminish. Generative AI models, however, maintain constant vigilance. They are trained to recognize the "latent space" of healthy anatomy; when a scan deviates from this norm, the AI flags it. These subtle anomalies often represent the earliest stages of disease, where intervention is most effective and least invasive.
Enhanced Image Reconstruction
Generative AI allows for "Sparse-view CT" and "Accelerated MRI." By taking fewer physical measurements (which reduces radiation exposure for the patient), the AI can "fill in the blanks" to generate a complete, high-quality diagnostic image. This not only makes the process safer but also significantly faster, reducing patient anxiety and wait times.
The Evolution of Image Analysis
Traditional image analysis was often qualitative—a radiologist looking at a film and describing what they saw. Today, Generative AI makes the process quantitative.
| Feature | Traditional Imaging | AI-Enhanced Imaging |
|---|---|---|
| Data Source | Raw sensor output | Reconstructed high-fidelity data |
| Processing | Manual measurement | Automated segmentation & quantification |
| Detection | Human-eye perception | Deep learning pattern matching |
| Speed | Minutes to hours | Seconds (Real-time) |
By integrating Generative AI into the workflow, hospitals are seeing a 20-30% increase in the detection of early-stage cancers. The AI provides a "heat map" of areas of interest, allowing the specialist to focus their expertise where it matters most.
Future Trends: 2026 and Beyond
As we move through 2026, the trend is shifting from "experimental pilots" to "infrastructure." Generative AI is becoming a standard feature in imaging hardware. We are seeing the rise of Agentic AI—systems that don't just flag a scan but also draft the initial radiology report, cross-reference the patient’s electronic health records (EHR), and suggest the next step in the clinical pathway.
Furthermore, Multi-modal LLMs (Large Language Models) are beginning to "look" at images and "read" clinical notes simultaneously. This allows for a holistic diagnosis that considers not just the pixel data but also the patient's symptoms, genetic history, and previous lab results.
Conclusion
The integration of Generative AI in diagnostic imaging is not about replacing the physician; it is about augmenting human capability. By utilizing deep learning to perform complex image analysis, medical AI allows for the early detection of subtle anomalies that save lives. As radiology moves into an AI-first era, the focus remains on the patient: faster scans, lower radiation, and more accurate diagnoses.