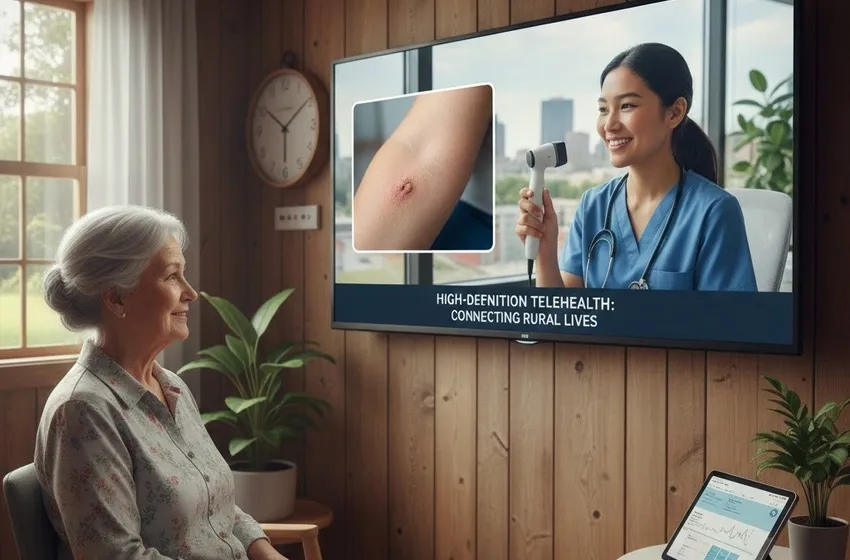
Discover how high-definition telehealth and virtual platforms are improving specialty care access
The Future of Equity: How Telemedicine is Bridging the Rural Specialty Care Gap
For decades, the "zip code" factor has been one of the most significant determinants of health outcomes. In rural America and other underserved regions globally, the distance between a patient and a medical specialist isn't just measured in miles—it's measured in months of waiting, hundreds of dollars in travel costs, and, tragically, the progression of treatable diseases. However, the paradigm is shifting. Through the strategic integration of Telemedicine, healthcare systems are finally dismantling the geographical barriers that once defined medical inequality.
By leveraging virtual platforms, healthcare providers are now able to bring specialty care access to the most remote corners of the map. From the precise visual requirements of dermatology to the nuanced, conversational needs of psychiatry, high-definition telehealth is proving that world-class medicine no longer requires a trip to the big city.
The Crisis of Rural Healthcare Access
Rural communities face a "triple threat" of healthcare challenges: an aging population with complex chronic needs, a shrinking pool of local providers, and a complete lack of specialized services. Statistics show that while 20% of the U.S. population resides in rural areas, only about 10% of physicians practice there.
When a patient in a remote town needs a specialist—be it for a suspicious skin lesion or a worsening mental health crisis—the "local" option often doesn't exist. This leads to:
- Delayed Diagnoses: Patients wait until symptoms are unbearable before seeking care due to travel burdens.
- Financial Strain: The cost of gas, lodging, and time off work makes remote consultations a financial necessity rather than a luxury.
- Provider Burnout: Local primary care physicians (PCPs) are often forced to manage complex conditions outside their scope because there is no one else to refer to.
High-Definition Telehealth: The Tech Behind the Transformation
The early days of video calls were often marred by grainy images and lagging audio—limitations that made certain specialties, like dermatology, nearly impossible to practice virtually. Today, high-definition telehealth has changed the game.
Advanced virtual platforms now offer 4K video resolution, specialized peripheral attachments (like digital otoscopes and dermascopes), and end-to-end encryption that meets strict HIPAA standards. This level of clarity allows a dermatologist in a metropolitan teaching hospital to examine a patient’s skin in a rural clinic with as much detail as if they were in the same room.
Spotlight: Teledermatology
Dermatology is a visual science. Through high-definition telehealth, clinicians can utilize "store-and-forward" technology or live video to:
- Screen for Malignancy: High-res images allow for the early detection of melanomas.
- Manage Chronic Conditions: Psoriasis and eczema treatments can be adjusted via frequent, low-friction remote consultations.
- Triage Urgency: Specialists can determine which cases require immediate biopsy and which can be managed locally, saving the patient unnecessary travel.
Psychiatry: Breaking Stigma and Distance
While dermatology requires high-visual fidelity, psychiatry relies on "the therapeutic alliance"—the connection and communication between patient and provider. In rural healthcare, mental health services are often the most scarce.
Telemedicine has been a revolutionary force in behavioral health for several reasons:
- Privacy and Comfort: Patients can attend sessions from their own homes, reducing the stigma often felt when walking into a local mental health clinic in a small town.
- Consistency of Care: In areas where psychiatric providers may rotate or visit only once a month, virtual platforms ensure a patient sees the same doctor every time.
- Crisis Intervention: Virtual access means a patient in a mental health crisis can reach a specialist in minutes rather than hours, potentially preventing emergency room visits or self-harm.
The Workflow: How Remote Consultations Work
The modern "Clinic-to-Clinic" model is the gold standard for expanding specialty care access. Instead of a patient navigating a complex app alone at home, they visit their local primary care office.
- Local Facilitation: A nurse or medical assistant at the rural clinic prepares the patient and sets up the high-definition telehealth equipment.
- The Virtual Exam: The specialist joins the call via a secure link. Using high-def cameras, they perform the exam, often guided by the local nurse who can use physical tools (like stethoscopes) that stream data directly to the specialist.
- Collaborative Care: The specialist, the local PCP, and the patient discuss the treatment plan together. This ensures that the local team is fully looped in for follow-up care, maintaining a "medical home" for the patient.
Overcoming the Digital Divide
Despite the promise of Telemedicine, the "Digital Divide" remains a hurdle. Rural healthcare expansion is only as strong as the local internet connection. To truly scale these services, two things are happening in 2025:
- Infrastructure Investment: Federal grants are prioritizing broadband expansion in "internet deserts."
- Hybrid Hubs: Large health systems are establishing "Telehealth Hubs" in community centers or libraries, ensuring that even those without a smartphone or home Wi-Fi can access remote consultations.
The Economic Impact of Virtual Platforms
The benefits of specialty care access aren't just clinical; they are economic. For rural hospitals, keeping care local is a matter of survival. When a patient is transferred to a city for specialty care, the rural hospital loses revenue. By using Telemedicine, the rural facility can keep the patient in their bed, provide the specialist's expertise virtually, and maintain the facility's financial health.
For the patient, the savings are immediate. A single remote consultation can save an average of $150 in travel costs and 4–6 hours of travel time. Over the course of a chronic treatment plan, this translates to thousands of dollars stayed in the pockets of rural families.
Conclusion: A New Era of Healthcare Equity
The expansion of specialty care access through high-definition telehealth is more than a technological trend; it is a moral imperative. By integrating Telemedicine into the fabric of rural healthcare, we are ensuring that quality of care is no longer dictated by geography.
As virtual platforms become more intuitive and remote consultations become the norm, the distinction between "rural" and "urban" medicine will begin to fade. In its place, we will find a unified healthcare system where a farmer in Iowa and a CEO in Manhattan have the same access to the world’s best dermatologists, psychiatrists, and specialists.