Learn the CAD definition, common angina symptoms, and the critical differences between stable and unstable angina in this guide to the most common heart disease.
Understanding Coronary Artery Disease and Angina: A Comprehensive Guide
The human heart is an incredible machine, beating approximately 100,000 times a day to pump life-sustaining blood to every corner of the body. However, for this pump to function, it needs a constant supply of oxygen-rich blood for itself. This is where the coronary arteries come into play. When these vital pathways are compromised, it leads to the most prevalent form of cardiovascular illness worldwide.
CAD Definition: The Silent Progression
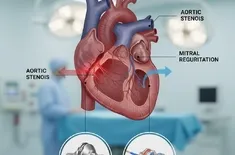
To begin, we must establish a clear CAD definition. Coronary Artery Disease (CAD) is a condition where the major blood vessels that supply the heart struggle to deliver enough blood, oxygen, and nutrients to the heart muscle. This struggle is almost always caused by a process called atherosclerosis—the gradual buildup of fats, cholesterol, and other substances (known as plaque) on the inner walls of the heart arteries.
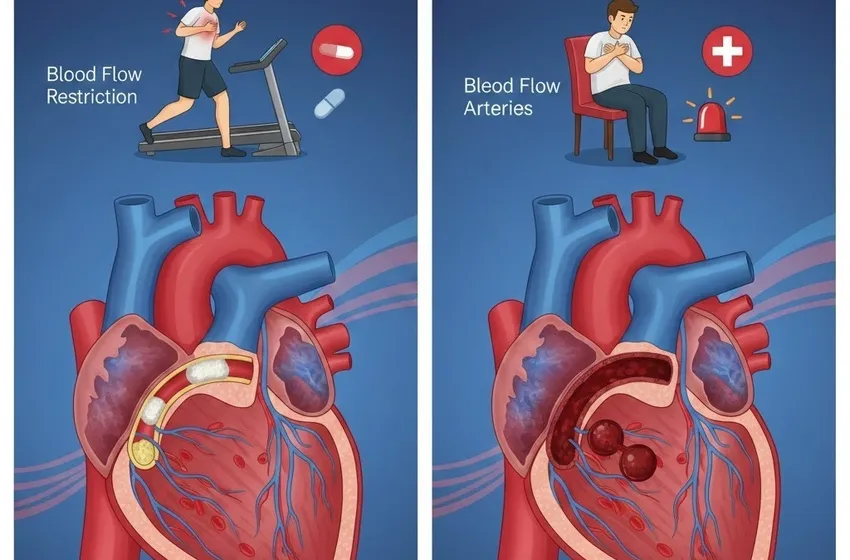
As this plaque accumulates over decades, it causes the arteries to narrow and harden. This blood flow restriction means that while your heart may get enough blood while you are sitting still, it cannot get the "boost" it needs when you are active or stressed. Because it develops slowly, many people do not realize they have CAD until they experience their first bout of chest pain or, more seriously, a heart attack. It is widely recognized by medical professionals as the most common type of heart disease, affecting millions and serving as a leading cause of mortality globally.
What is Angina? The Heart’s Warning Signal
If CAD is the underlying disease, angina is its primary symptom. Angina is not a disease itself; rather, it is the pain or discomfort that occurs when your heart muscle isn't getting enough oxygen-rich blood. Think of it as a "cramp" in the heart muscle.
While most people associate heart issues with a sharp "stabbing" sensation, angina symptoms are often more nuanced. Common descriptions include:
- A feeling of heavy pressure or squeezing.
- A sensation of fullness or "indigestion" in the chest.
- Tightness that may radiate to the jaw, neck, back, or arms.
- Shortness of breath and unexplained fatigue.
Identifying Different Chest Pain Types
Not all chest pain is created equal. When evaluating heart health, doctors categorize chest pain types to determine the severity of the blockage and the immediate risk to the patient.
- Stable Angina: This is the most common form. It occurs when the heart is working harder than usual (such as during exercise or climbing stairs) and follows a predictable pattern.
- Unstable Angina: This is a much more dangerous situation. It does not follow a pattern and can happen even when you are resting.
- Variant (Prinzmetal’s) Angina: A rare form caused by a spasm in the coronary arteries rather than a blockage.
- Microvascular Angina: Pain caused by malfunctions in the smallest blood vessels of the heart.
Stable Angina: The Predictable Pattern
Stable angina is typically chronic and manageable. It occurs when the heart's demand for oxygen exceeds the supply available through narrowed arteries.
The Trigger: Usually physical exertion, emotional stress, or even a heavy meal. The Duration: It typically lasts a short time (5 minutes or less). The Relief: The pain goes away promptly with rest or by taking a prescription medication like nitroglycerin, which widens the blood vessels. The Outlook: While it indicates significant CAD, it is not an immediate heart attack. However, it requires lifestyle changes and medical management to prevent it from worsening.
Unstable Angina: The Medical Emergency
Unlike its stable counterpart, unstable angina is unpredictable and signals that a heart attack may be imminent. This usually happens because a plaque buildup has ruptured, causing a blood clot to form and suddenly increase the blood flow restriction.
The Trigger: There is often no trigger; it can happen while sitting, watching TV, or sleeping. The Duration: The pain is more severe and lasts longer than stable angina (often 20 minutes or more). The Relief: Resting or taking medication does not make the pain go away. The Outlook: This is a medical emergency. If you experience chest pain that is new, different, or worsening, you must seek emergency care immediately.
Comparison Table
| Feature | Stable Angina | Unstable Angina |
|---|---|---|
| Predictability | Predictable pattern | Unpredictable; new or different |
| Trigger | Physical exertion or stress | Often occurs at rest |
| Duration | Short (1–5 minutes) | Long (20 minutes) |
| Relief | Relieved by rest/nitroglycerin | Not relieved by rest/meds |
| Urgency | Non-emergency (needs monitoring) | Emergency (Seek help now) |
Risk Factors and Prevention
Since CAD is a progressive disease, understanding your risks is the first step in prevention. Major risk factors include:
- High Blood Pressure & Cholesterol: These damage the artery walls, making it easier for plaque to stick.
- Smoking: Chemicals in tobacco damage heart arteries and increase the risk of clots.
- Diabetes: High blood sugar can damage the nerves and blood vessels that control the heart.
- Sedentary Lifestyle: Lack of exercise contributes to obesity and poor vascular health.
Conclusion
Understanding the link between CAD definition, the anatomy of heart arteries, and the resulting angina symptoms is vital for long-term health. While Coronary Artery Disease is the most common type of heart disease, it is also largely manageable through early detection and lifestyle shifts. Recognizing the difference between the "warning light" of stable angina and the "red alert" of unstable angina can quite literally be the difference between life and death.