Discover effective lifestyle interventions to manage high blood pressure without medication.
Managing High Blood Pressure Naturally: Your Guide to Lifestyle Intervention
High blood pressure, or hypertension, is often called the "silent killer" because it frequently has no obvious symptoms while significantly increasing the risk of heart disease and stroke. If you have been diagnosed with "elevated" blood pressure or Stage 1 hypertension, your doctor may suggest a window of lifestyle intervention before turning to pharmacological solutions.
The good news is that the cardiovascular system is incredibly responsive to behavioral changes. By implementing actionable, evidence-based natural methods, many individuals can manage mildly elevated blood pressure before pharmacological intervention is necessary.
The Foundation: Salt Reduction
The link between sodium intake and hypertension is one of the most well-established facts in cardiovascular medicine. Salt reduction is critical because when you consume too much salt, your body retains extra water to wash the salt out. This extra water increases your total blood volume, which puts more pressure on your blood vessel walls.
- Read Labels: Roughly 75% of dietary sodium comes from processed and restaurant foods.
- The Rule of 1500: While the general recommendation is under 2,300mg per day, those with elevated blood pressure often see significant results by aiming for 1,500mg.
- Flavor Alternatives: Use lemon juice, vinegars, and fresh herbs to season food instead of sodium-heavy spice blends.
The Power of Potassium and Magnesium
While lowering sodium is vital, increasing your intake of specific minerals is equally important. Potassium and magnesium act as natural vasodilators, helping blood vessels relax and improving the body’s ability to excrete excess sodium.
Potassium eases tension in your blood vessel walls (found in bananas and spinach), while magnesium helps regulate enzyme systems that control blood pressure (found in seeds and leafy greens).
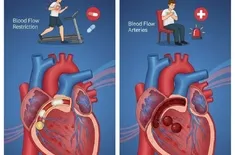
Prioritizing Aerobic Exercise
Physical activity is perhaps the most potent non-drug prescription available. Engaging in regular aerobic exercise strengthens the heart, allowing it to pump more blood with less effort. When the heart works less, the force on your arteries decreases.
Aim for at least 150 minutes of moderate-intensity activity per week, such as brisk walking, cycling, or swimming, to benefit from the post-exercise hypotension effect.
Understanding Caffeine Effects
The relationship between caffeine and blood pressure is nuanced. For some, caffeine causes a short-term, dramatic spike in blood pressure. While the long-term caffeine effects on chronic hypertension are still debated, those who are caffeine sensitive may experience persistent elevations and should monitor their readings after consumption.
Alcohol Moderation
Alcohol can be both a short-term and long-term trigger for hypertension. Alcohol moderation is defined as no more than one drink a day for women and two for men. Exceeding these limits can reduce the effectiveness of blood pressure treatments and cause weight gain.
Stress Management and Deep Breathing
Stress triggers the release of hormones that constrict blood vessels. Practicing deep breathing exercises, such as the 4-7-8 technique, can activate the parasympathetic nervous system, which acts as a brake for your stress response and helps lower systolic pressure over time.
Summary of Natural Methods
| Method | Impact on Systolic BP (Approx) |
|---|---|
| Weight Loss | 1 mmHg per kg lost |
| DASH Diet | 8–14 mmHg |
| Aerobic Exercise | 5–8 mmHg |
| Salt Reduction | 2–8 mmHg |
| Alcohol Moderation | 2–4 mmHg |