Discover how to navigate recovery after a heart attack or heart surgery.
Recovering with Confidence: Your Comprehensive Guide to Cardiac Rehabilitation
Undergoing a major heart event—whether it’s a heart attack, stent placement, or bypass surgery—is a life-altering experience. It’s natural to feel a mix of relief and uncertainty about the future. You might wonder, “How much can I safely move?” or “Will my heart ever be strong again?”
This is where a cardiac rehabilitation program becomes your most valuable asset. Far from being just a gym membership for heart patients, it is a medically supervised, multidisciplinary roadmap designed to help you reclaim your health.
Understanding Cardiac Rehabilitation
Cardiac rehabilitation is a structured program involving medical evaluation, supervised exercise, patient education, and emotional support. Its primary goal is to improve your cardiovascular health and quality of life while reducing the risk of future heart problems.
Who is it for?
Rehab is recommended for individuals who have experienced:
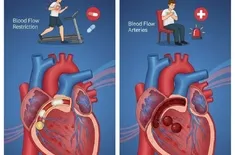
- Heart attack (Myocardial Infarction)
- Coronary artery bypass graft (CABG)
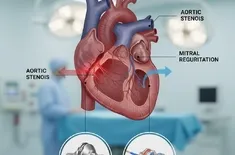
- Heart valve repair or replacement
- Stable angina
- Heart failure
- Heart transplant
The Four Cardiac Rehab Stages
Recovery is not a sprint; it’s a progression. To ensure safety and effectiveness, the program is typically divided into four distinct cardiac rehab stages.
Stage I: The Clinical Phase (Inpatient)
This stage begins while you are still in the hospital. The focus is on basic mobility and assessing your readiness for discharge.
- Physical Activity: Gentle tasks like sitting up in bed, standing, and walking short distances in the hallway.
- Education: Nurses and therapists provide initial patient education on your diagnosis, the medications you’ve been prescribed, and warning signs to watch for at home.
- Discharge Planning: Your team will discuss what you can and cannot do during your first week at home.
Stage II: The Outpatient Monitoring Phase
This is the "core" of the program, usually starting 2 to 6 weeks after hospital discharge. You will visit a rehab facility several times a week.
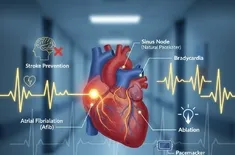
- Continuous Monitoring: During supervised exercise sessions, you will wear an EKG (electrocardiogram) monitor so staff can track your heart rhythm and blood pressure in real-time.
- Duration: Typically lasts 3 to 12 weeks, depending on your insurance and clinical needs.
Stage III: The Intermediate Phase (Maintenance)
Once you have demonstrated that your heart responds well to exertion, the intensive monitoring (EKG leads) is usually removed.
- Independence: You continue your exercise routine under the watchful eye of the staff, but with more personal responsibility for monitoring your own intensity.
- Focus: Transitioning the habits learned in Stage II into a long-term lifestyle.
Stage IV: The Maintenance Phase (Life-Long)
This is the final, indefinite stage of recovery after heart attack or surgery. It involves self-monitored exercise and permanent adherence to heart-healthy habits. Many patients choose to continue exercising in a community or clinical setting for the social support and specialized equipment.
Core Components of the Program
1. Supervised Exercise: The Engine of Recovery
Exercise is the "medicine" of cardiac rehab. Many patients fear that overexerting themselves will cause another heart event. Supervised exercise eliminates that fear by ensuring every movement is within a safe target heart rate zone.
- Aerobic Conditioning: Walking on treadmills, using stationary bikes, or rowing machines to strengthen the heart muscle.
- Strength Training: Using light weights or resistance bands to improve overall metabolic health.
- Flexibility: Stretching to improve circulation and reduce the physical stress on the body.
2. Patient Education: Knowledge is Power
Understanding the "why" behind your treatment is crucial for long-term success. Patient education covers a broad spectrum of topics:
- Medication Management: Understanding how beta-blockers, statins, and anti-platelets work together to protect your heart.
- Symptom Recognition: Learning the difference between "good" exercise fatigue and "bad" cardiac symptoms.
3. Lifestyle Coaching: Redefining Daily Habits
The habits that led to a heart event must be addressed to prevent a recurrence. Lifestyle coaching involves working with dietitians and specialists to:
- The Heart-Healthy Diet: Moving toward a Mediterranean or DASH-style eating plan.
- Smoking Cessation: Providing tools and support to quit tobacco, which is perhaps the single most important step for heart health.
- Weight Management: Setting realistic goals to reduce the strain on your cardiovascular system.
4. Emotional Support: Healing the Mind
It is often said that when the heart is wounded, the mind follows. Anxiety and depression are incredibly common following a cardiac event. Emotional support through counseling or peer groups is a vital part of the healing process.
A Step-by-Step Guide for Patients
If you are about to start your journey, here is what your first few weeks will look like:
Step 1: The Initial Assessment
Before you touch a treadmill, you will have a 1-on-1 meeting with a rehab specialist. They will review your medical history, perform a physical exam, and create your baseline.
Step 2: Goal Setting
Your team will ask you what you want to achieve. For some, it’s returning to work; for others, it’s being able to pick up their grandchildren. Your program is tailored to these personal milestones.
Step 3: The Routine
You will typically attend sessions 2–3 times per week. Each session follows a pattern of check-in, warm-up, the work phase, cool-down, and an educational seminar.
Step 4: Periodic Re-evaluation
Every few weeks, your progress is measured. As your heart becomes more efficient, your exercise prescription will be adjusted to continue your improvement.
Overcoming Common Barriers
Despite the proven benefits, many patients hesitate to join or finish rehab. Facilities often offer flexible hours to accommodate time constraints, and insurance providers like Medicare typically cover Stage II rehab for qualifying diagnoses.
Why It Matters: The Long-Term Impact
The statistics are clear: patients who complete a cardiac rehabilitation program have a 25% to 30% lower risk of fatal heart events compared to those who do not. By engaging in cardiac rehab stages, embracing supervised exercise, and soaking up patient education, you aren't just surviving a heart event—you are building a stronger, more resilient version of yourself.