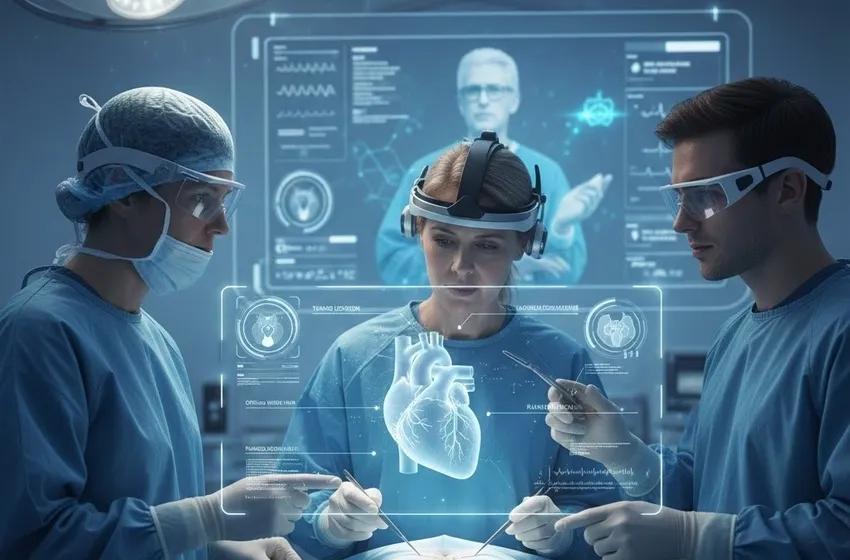
Discover how AR medical training uses 3D anatomical visualization and real-time surgical guidance to enhance learning and improve outcomes in medical education.
The Future of Medicine: How Augmented Reality is Revolutionizing Medical Training
The landscape of healthcare is undergoing a radical transformation, driven by the integration of cutting-edge technology. Among these innovations, AR medical training stands out as a bridge between theoretical knowledge and clinical mastery. By merging digital data with the physical world, Augmented Reality (AR) offers a solution to the long-standing challenges of traditional medical education, such as limited access to cadavers and the high-risk nature of learning on live patients.
What is Augmented Reality in Healthcare?
Augmented Reality is a technology that overlays computer-generated information—including 3D models, data visualizations, and text—onto a user's real-world environment. Unlike Virtual Reality (VR), which creates a completely synthetic world, AR keeps the user grounded in reality while providing a "digital layer" of insight. In a clinical setting, this means a surgeon can see a patient's internal anatomy projected directly onto their skin during an operation, or a student can visualize the blood flow through a heart while looking at a physical mannequin.
Transforming Anatomical Visualization
One of the most significant hurdles in early medical schooling is the transition from 2D textbook diagrams to the 3D complexity of the human body. Anatomical visualization through AR solves this by allowing students to interact with hyper-realistic, three-dimensional models.
- Layer-by-Layer Exploration: Students can use AR headsets or tablets to peel back layers of skin, muscle, and bone. This depth of interaction helps them understand the spatial relationships between organs.
- Pathology Interaction: Rather than just seeing a healthy heart, trainees can toggle between various conditions, such as atherosclerosis, observing how these pathologies change the organ's function in real-time.
- Accessible Learning: AR eliminates the dependency on expensive and scarce cadavers. With enhanced learning tools, a student in a remote location can access the same high-fidelity anatomical models as a student at a top-tier university.
Real-Time Surgical Guidance
The operating room is a high-stakes environment where precision is everything. AR is revolutionizing this space by providing surgical guidance that was previously unimaginable.
Using AR Overlays to Guide Complex Procedures
During a procedure, a surgeon can wear an optical see-through head-mounted display (HMD) that projects patient-specific data—such as CT or MRI scans—directly onto the surgical site. This "X-ray vision" allows the surgeon to:
- Map Incisions: Precisely locate tumors or vascular malformations before making the first cut.
- Avoid Critical Structures: View the exact path of nerves and blood vessels to prevent accidental damage.
- Real-Time Navigation: Track surgical instruments in relation to the patient's internal anatomy, ensuring that deep-tissue procedures are performed with sub-millimeter accuracy.
Creating a Safe Haven for Enhanced Learning
The "see one, do one, teach one" model of medical training is being replaced by a more robust "simulate many times before you do" approach. AR provides a risk-free environment where mistakes become valuable lessons rather than life-threatening errors.
- Repeatable Simulations: Trainees can practice complex techniques, such as spinal surgery or needle biopsies, hundreds of times. The system provides immediate feedback on their performance.
- Confidence Building: By mastering the movements in a simulated environment, residents enter the real operating room with higher confidence.
- Remote Mentorship: Using AR, an expert surgeon can provide real-time, "over-the-shoulder" guidance to a trainee in another part of the world using digital annotations.
The Rise of Mixed Reality (MR) in the Classroom
As we look toward 2026, the boundaries between AR and VR are blurring into what we call mixed reality. In this environment, digital objects not only appear in the real world but can be interacted with as if they were physical.
In medical education, this means students can collaborate around a shared holographic patient. They can "pull out" an organ to examine it, perform a virtual incision, and see how the body responds to different treatments. This level of immersion fosters a deep, intuitive understanding of physiology that traditional lectures simply cannot match.
Key Statistic: Research indicates that AR-assisted surgical training can reduce error rates by up to 21% and significantly shorten the learning curve for complex minimally invasive procedures.
Challenges and the Path Forward
While the benefits are clear, the widespread adoption of AR in medicine faces a few hurdles: hardware comfort, data integration for real-time imaging, and the initial cost of high-end systems. However, with the rapid advancement of 5G and AI-enhanced rendering, these challenges are being overcome.
Conclusion
AR medical training is no longer a futuristic concept—it is a current reality that is saving lives. From the initial stages of anatomical visualization to providing critical surgical guidance in the OR, this technology is the cornerstone of a new era in medical education. By fostering enhanced learning through mixed reality, we are empowering the next generation of doctors with the tools they need to perform with unprecedented precision.
``` Would you like me to generate the semantic keyword list and SEO tags as a separate text file or table?