Learn why an annual eye exam is vital for preventive care.
Diabetes and Your Eyes: What Retinopathy Looks Like
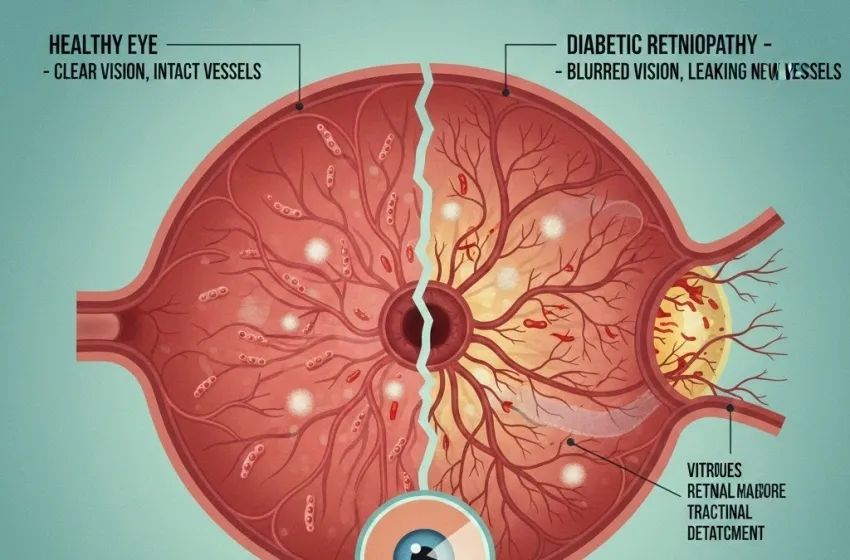
Diabetes is a systemic disease, meaning it affects the entire body. While many people focus on blood sugar management, cardiovascular health, or kidney function, the eyes are often overlooked until a problem arises. However, high blood sugar levels can wreak havoc on the delicate structures of the eye, leading to a condition called diabetic retinopathy. This condition is the leading cause of new cases of blindness among adults aged 20–74 years in the United States, and understanding its progression and the critical need for preventive care is paramount to preserving your sight.
The core problem in diabetic retinopathy lies in the microvascular damage—the destruction of the tiny blood vessels—that supply the retina. The retina is a light-sensitive layer of tissue at the back of the eye. It works much like the film in a camera (or the sensor in a digital one), converting light into electrical signals that the brain interprets as vision. When the blood vessels that nourish the retina are damaged by chronic high glucose, the entire visual system is put at risk.
The Silent Threat: How Uncontrolled Blood Sugar Damages Your Vision
The damage caused by diabetes to the blood vessels in the retina is insidious, meaning it develops slowly and often without immediate noticeable effects. This is why many people with diabetes don't realize they have a problem until the condition has advanced significantly, leading to potential vision loss.
High blood glucose causes a number of detrimental changes in the tiny blood vessels:
-
Vessel Weakening and Swelling: The walls of the capillaries in the retina become weak and begin to bulge, forming tiny balloon-like pouches called microaneurysms. These can leak fluid and blood into the retinal tissue.
-
Vessel Blockage: The blood vessels can become completely blocked, preventing the necessary supply of oxygen and nutrients from reaching the retina. Areas starved of oxygen (ischemia) trigger a cascade of destructive processes.
-
Abnormal New Vessel Growth (Proliferative Stage): In response to the lack of oxygen, the retina attempts to grow new blood vessels. This is a desperate attempt to restore circulation, but these new vessels are fragile, grow along the retinal surface and into the vitreous gel, and are prone to bleeding, scarring, and subsequent retinal detachment.
This progression, from mild damage to severe, highlights why early detection is crucial. In its initial stages, early symptoms of diabetic retinopathy—or lack thereof—are what make the condition so dangerous.
What Retinopathy Looks Like: Illustrating the Stages of Damage
To truly grasp the danger of uncontrolled blood sugar, it's essential to understand the four main stages of diabetic retinopathy.
1. Mild Non-Proliferative Diabetic Retinopathy (NPDR)
This is the earliest stage. The primary feature is the presence of microaneurysms. These are small areas of balloon-like swelling in the retinal capillaries. At this point, the patient usually has no noticeable vision loss or symptoms. This is a critical stage for intervention, as tight blood sugar and blood pressure control can halt the progression.
2. Moderate Non-Proliferative Diabetic Retinopathy (NPDR)
As the disease progresses, more blood vessels become blocked or damaged. The retina shows increased microaneurysms, hemorrhages (small bleeding spots), and "cotton-wool spots" (areas of retinal swelling from blocked vessels). Although vision may still be functional, the risk of developing macular edema (swelling of the central retina) increases significantly.
3. Severe Non-Proliferative Diabetic Retinopathy (NPDR)
This stage is marked by extensive bleeding and blockage of blood vessels. The retina is experiencing widespread oxygen deprivation (ischemia). The eye begins to produce growth factors, primarily Vascular Endothelial Growth Factor (VEGF), in a desperate signal to grow new blood vessels to compensate for the oxygen shortage. This severe oxygen deprivation is the precursor to the most serious stage.
4. Proliferative Diabetic Retinopathy (PDR)
This is the most advanced and sight-threatening stage. The growth factors released in the severe stage trigger the proliferation (growth) of abnormal, fragile new blood vessels on the surface of the retina and optic nerve—a process called neovascularization.
-
Vitreous Hemorrhage: These new vessels are easily broken and bleed into the vitreous gel (the clear, jelly-like substance that fills the eye), causing sudden, severe vision loss.
-
Tractional Retinal Detachment: As the neovascular tissue and associated scar tissue contract, they tug on the retina, potentially pulling it away from its underlying support structure. This is a surgical emergency that can lead to permanent blindness.
The Critical Importance of the Annual Eye Exam
Given that the most destructive forms of diabetic retinopathy often begin without early symptoms, relying on a change in vision is a dangerous approach. By the time a person notices blurring or vision changes, the damage is often extensive and more difficult to treat.
This underscores the non-negotiable requirement for an annual eye exam, specifically a dilated eye exam, for every person with diabetes.
What Happens During a Dilated Eye Exam?
During this specialized examination, the eye doctor (ophthalmologist or optometrist) puts drops into the eyes to widen (dilate) the pupils. This allows them a clear, wide-angle view of the retina and the optic nerve, providing the only way to detect the subtle, microscopic signs of microvascular damage before they impact vision.
The doctor looks for:
-
Microaneurysms and hemorrhages.
-
Signs of macular edema (swelling).
-
Evidence of vessel blockages (cotton-wool spots).
-
The growth of abnormal new blood vessels (neovascularization).
If signs of NPDR are detected, the doctor can establish a baseline and recommend closer follow-up, potentially moving from an annual schedule to exams every six months. Crucially, they can intervene with treatments like laser therapy or injections of anti-VEGF medication to manage the condition before PDR or severe vision loss occurs.
Treatment and Preventive Care: Taking Control
While advanced diabetic retinopathy requires specialized treatment, the best approach is always preventive care.
Pillars of Prevention:
-
Tight Glucose Control (A1C): Maintaining blood sugar levels within the target range set by your healthcare provider is the single most effective way to prevent or delay the onset and progression of the condition. Reducing your HbA1c level is directly correlated with a decreased risk of developing microvascular damage.
-
Blood Pressure Management: High blood pressure (hypertension) significantly accelerates the development and worsening of diabetic retinopathy. Keeping blood pressure under control is just as vital as managing blood glucose.
-
Cholesterol Management: Elevated blood lipids contribute to the formation of hard, fatty deposits (exudates) in the retina, worsening vision loss.
-
No Smoking: Smoking severely constricts blood vessels and exacerbates existing microvascular damage, rapidly speeding up the progression of the disease.
Treatment Options for Advanced Retinopathy:
For those who have progressed to severe NPDR or PDR, treatment options are highly effective:
-
Anti-VEGF Injections: Medications that block the action of Vascular Endothelial Growth Factor (VEGF) are injected into the eye. These powerful drugs cause the abnormal new blood vessels to shrink and regress, reducing leakage and swelling.
-
Laser Treatment (Photocoagulation): Focused laser light is used to seal leaking blood vessels or to strategically destroy peripheral areas of the retina. This reduces the oxygen demand and stops the retina from signaling for the growth of more abnormal vessels.
-
Vitrectomy: In cases of severe vitreous hemorrhage or tractional retinal detachment, a surgeon can remove the blood-filled vitreous gel and scar tissue, allowing light to reach the retina once again.
The connection between diabetes and your eyes is direct and undeniable. Understanding what retinopathy looks like, from the microscopic microvascular damage of its early symptoms to the catastrophic bleeding of PDR, should serve as a powerful motivator. Commitment to an annual eye exam and rigorous preventive care is the only way to safeguard your long-term vision against the complications of diabetic retinopathy. Your sight is precious; take the proactive steps necessary to protect it.