Discover why heart disease is rising in young adults.
Heart Disease in Young Adults: Causes and Prevention
For decades, heart disease was viewed almost exclusively as a condition of the elderly. However, the medical landscape has shifted dramatically in the 2020s. Today, clinicians are witnessing a concerning spike in cardiovascular events among people in their 20s and 30s. Addressing the rising trend of heart issues in younger populations is no longer just a medical necessity; it is a public health emergency.
While traditional risk factors like obesity and sedentary lifestyles remain prevalent, new-age variables such as vaping effects, the use of performance enhancers, and a surge in substance abuse risk are rewriting the narrative of cardiac health. Understanding the complex interplay between lifestyle choices and undiagnosed congenital issues is the first step toward reclaiming heart health for the next generation.
The New Profile of Heart Disease: Why the Shift?
Statistical updates for 2025 reveal that nearly 1 in 5 heart attack patients are now under the age of 40. This shift is driven by a "perfect storm" of high-stress environments, evolving consumption habits, and a historic lack of screening in younger demographics.
Many young adults operate under the "invincibility myth"—the belief that they are too young for heart trouble. This often leads to a delay in seeking medical attention for symptoms like chest discomfort or shortness of breath. By the time a diagnosis is made, the damage may already be extensive.
Key Causes of Heart Disease in Young Adults
1. Substance Abuse Risk and Stimulant Use
One of the most significant contributors to the rising young adult heart risk is the use of stimulants. This includes both illicit substances like cocaine and methamphetamines, as well as the misuse of prescription medications for ADHD or performance enhancement.
- Physiological Impact: Stimulants cause an immediate, sharp increase in heart rate and blood pressure. They can trigger coronary artery spasms, leading to a myocardial infarction even in a heart with no prior plaque buildup.
- Long-term Damage: Chronic use can lead to the thickening of the heart walls and permanent arrhythmias, significantly increasing the substance abuse risk associated with cardiac failure.
2. The Hidden Danger: Vaping Effects
For years, e-cigarettes were marketed as a "safer" alternative to smoking. However, recent research highlights severe vaping effects on the cardiovascular system.
- Endothelial Dysfunction: The aerosolized chemicals in vapes damage the lining of blood vessels (the endothelium), making them stiff and prone to inflammation.
- Nicotine Toxicity: High concentrations of nicotine in flavored pods can cause "electrical storms" in the heart, potentially leading to lethal rhythm disturbances.
3. Undiagnosed Congenital Defects
Not all heart issues are self-inflicted. A substantial portion of the young adult heart risk stems from congenital defects that went undetected during childhood.
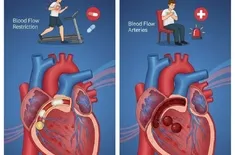
- Hypertrophic Cardiomyopathy (HCM): This genetic condition causes the heart muscle to become abnormally thick, making it harder for the heart to pump blood. It is a leading cause of sudden cardiac arrest (SCA) in young athletes.
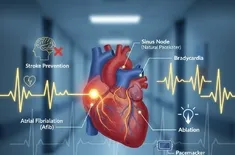
- Brugada Syndrome and Long QT Syndrome: These are electrical abnormalities that do not show up on standard physicals but can be identified through early diagnosis and targeted ECG screenings.
Understanding the Threat of Sudden Cardiac Arrest (SCA)
Perhaps the most terrifying manifestation of heart disease in youth is sudden cardiac arrest (SCA). Unlike a heart attack, which is a "plumbing problem" caused by a blockage, SCA is an "electrical problem" where the heart suddenly stops beating.
Without immediate intervention via CPR or an Automated External Defibrillator (AED), SCA is almost always fatal. For young adults, the risk of SCA is often tied to a combination of high-intensity physical exertion and an underlying, often undiagnosed, heart condition.
Prevention Strategies for the Modern Young Adult
Prevention is the most powerful tool in the fight against early-onset heart disease. It requires a proactive approach that combines lifestyle modifications with clinical vigilance.
The Power of Early Diagnosis
The "wait and see" approach is dangerous. Early diagnosis through routine check-ups can catch hypertension and high cholesterol before they cause permanent arterial damage.
- Know Your Numbers: Every adult over 20 should know their blood pressure, LDL cholesterol, and fasting blood glucose levels.
- Screening for Congenital Issues: If you have a family history of sudden death or if you experience unexplained fainting, a specialized cardiac screening (including an ECG and echocardiogram) is essential to rule out congenital defects.
Lifestyle as Medicine
The American Heart Association's "Life’s Essential 8" provides a roadmap for reducing young adult heart risk:
- Eat Better: Focus on whole foods, lean proteins, and healthy fats while minimizing processed sugars.
- Be More Active: Aim for at least 150 minutes of moderate-intensity aerobic activity per week.
- Quit Tobacco and Vapes: Eliminating nicotine is the single most effective way to improve vascular health.
- Manage Weight: Reducing strain on the heart by maintaining a healthy BMI.
- Get Healthy Sleep: Poor sleep is linked to high cortisol and increased heart rate.
Navigating the Psychological Factors: Stress and Heart Health
The "hustle culture" of the 2020s has placed unprecedented psychological strain on young adults. Chronic stress triggers a constant "fight or flight" response, flooding the body with adrenaline and cortisol. This state of chronic inflammation is a direct precursor to atherosclerosis (hardening of the arteries).
| Stressor | Impact on Heart | Mitigation Strategy |
|---|---|---|
| High-Pressure Career | Chronic Hypertension | Boundary setting & Mindfulness |
| Social Media Comparison | Increased Anxiety/Palpitations | Digital detoxing |
| Sleep Deprivation | Arrhythmia Risk | Strict sleep hygiene (7-9 hours) |
Conclusion: Taking Charge of Your Cardiac Future
The rising tide of heart disease in the younger population is a call to action. By recognizing the severe vaping effects, managing the substance abuse risk, and seeking early diagnosis for potential congenital defects, young adults can significantly alter their health trajectory.
Protecting your heart is not about making one-time changes; it’s about a sustained commitment to health. Whether it's through regular exercise, better nutrition, or advocating for your own medical screenings, the time to act is now—before a silent issue becomes a life-threatening crisis.