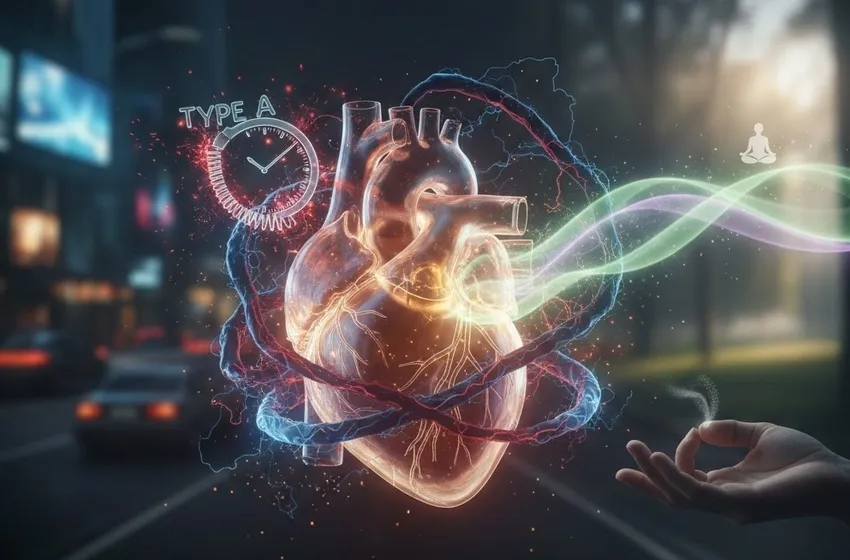
Learn about inflammation, Type A risks, and proven mindfulness techniques for relief.
Stress and Anxiety: How They Damage Your Heart
We often think of heart disease as a byproduct of poor diet and a sedentary lifestyle. While those factors are critical, there is a silent, invisible architect of cardiovascular decay: chronic stress. The connection between our emotional state and our arterial health is not just metaphorical; it is a complex biological reality.
The Biology of the "Broken Heart": The Physiological Pathway
When we experience a perceived threat, our body’s "fight or flight" system kicks in. While this was useful for escaping predators, the modern world keeps this system perpetually "on."
The Cortisol Cascade
Under chronic stress, the adrenal glands continuously pump out hormones like adrenaline and cortisol. Cortisol effects are particularly damaging when sustained. While cortisol is necessary for regulating metabolism and immune response in short bursts, its long-term presence acts like a slow-acting toxin to the vascular system.
The Mechanism of Damage
- Increased Blood Pressure: Adrenaline increases your heart rate and tightens blood vessels. Over time, this constant pressure creates micro-tears in the arterial walls.
- Systemic Inflammation: One of the most dangerous aspects of long-term stress is inflammation. Chronic cortisol exposure can lead to "glucocorticoid receptor resistance," meaning the body can no longer turn off the inflammatory response. This inflammation promotes the buildup of plaque in the arteries (atherosclerosis).
- Blood Clotting: Stress makes blood stickier. In an evolutionary sense, this prevented us from bleeding out during a hunt. In the modern office, it simply increases the risk of a heart attack or stroke.
The "Type A" Factor: Personality and Cardiovascular Risk
In the 1950s, cardiologists identified what they called the Type A personality. This profile describes individuals who are highly competitive, ambitious, impatient, and prone to hostility.
While ambition is generally praised, the "hostility" component of the Type A profile is a significant predictor of cardiovascular risk. Those who react to daily inconveniences with intense anger or cynicism experience sharper spikes in blood pressure and higher levels of pro-inflammatory cytokines, making their hearts more vulnerable to sudden events.
How Anxiety Directly Impacts Heart Rhythm
Anxiety isn't just "worry"; it is a physical state. People with generalized anxiety disorder (GAD) often have lower heart rate variability (HRV). HRV is a measure of the variation in time between each heartbeat. A high HRV means your nervous system is flexible and healthy; a low HRV—common in anxious individuals—indicates that the body is stuck in a stressed state, making the heart less resilient to physical or emotional demands.
Actionable Coping Strategies: Protecting Your Arteries
Understanding the damage is the first step, but mitigation is where the healing begins. Implementing stress reduction techniques can physically alter your biochemistry and lower your heart rate.
1. The Power of Mindfulness
Mindfulness is the practice of maintaining a non-judgmental awareness of the present moment. Research shows that consistent mindfulness meditation can:
- Lower resting heart rate.
- Reduce serum cortisol levels.
- Decrease the "reactivity" of the amygdala (the brain's fear center).
2. Vagus Nerve Stimulation
The vagus nerve is the "reset button" for your nervous system. You can stimulate it through:
- Deep Diaphragmatic Breathing: Inhaling for 4 seconds, holding for 4, and exhaling for 8. This signals the brain to move from the sympathetic (stress) to the parasympathetic (rest) nervous system.
- Cold Exposure: Splashing cold water on your face can trigger the "mammal dive reflex," which naturally slows the heart.
3. Physical Activity as a Buffer
Exercise is a paradox: it creates short-term stress to provide long-term resilience. Regular aerobic exercise helps the body process cortisol effects more efficiently and strengthens the heart muscle so it doesn't have to work as hard during emotional stressors.
Creating a "Heart-Centric" Lifestyle
To truly combat the effects of stress, one must look beyond the gym and the kitchen.
- Sleep Hygiene: Sleep is when the heart repairs itself. Chronic sleep deprivation is a major source of inflammation.
- Social Connection: Strong social ties are linked to lower blood pressure. Isolation, conversely, is as significant a risk factor for heart disease as smoking.
- Boundaries: For the Type A personality, learning to say "no" is a medical necessity. Reducing your cognitive load reduces your cardiac load.
Final Thoughts
Your heart is more than a pump; it is a sensitive instrument that reacts to every emotion you feel. By addressing chronic stress through intentional stress reduction techniques, you aren't just "relaxing"—you are actively performing preventative medicine. Whether it's through mindfulness, better sleep, or managing a Type A personality, your heart deserves a break.