The Hidden Cardiovascular Risks
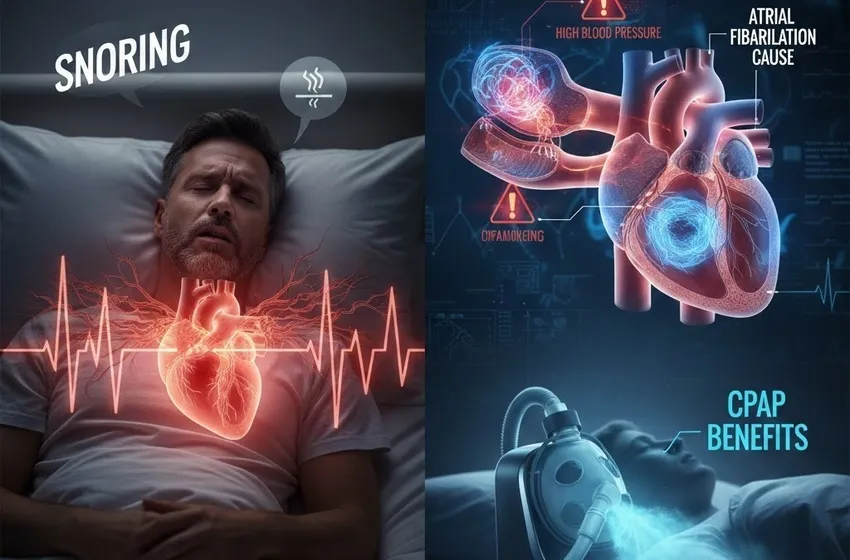
Sleep Apnea’s Hidden Risk to Your Cardiovascular Health: The Silent Strain on Your Heart
When we think of sleep apnea, we often think of it as a nuisance—loud snoring, daytime fatigue, or perhaps a partner’s complaint about restless nights. However, beneath the surface of interrupted sleep lies a much more sinister reality. There is a profound and dangerous sleep apnea link to cardiovascular disease that remains one of the most overlooked health crises in modern medicine.
For millions of people, sleep apnea isn’t just a sleep disorder; it is a chronic cardiovascular stressor. The repeated cycles of breathlessness and gasping for air do more than just ruin your morning; they physically reshape the health of your heart and blood vessels.
The Invisible Mechanism: How Oxygen Deprivation Damages the Heart
At the core of obstructive sleep apnea (OSA) is a physical blockage of the airway. When the muscles in the throat relax excessively, the airway collapses, leading to episodes of oxygen deprivation (hypoxemia).
When your blood oxygen levels drop, your body enters a "fight or flight" state. The brain senses the lack of oxygen and sends a panicked signal to the sympathetic nervous system. This triggers a massive release of adrenaline and cortisol, forcing the heart to beat faster and the blood vessels to constrict to keep the brain alive.
This process doesn't happen just once. In severe cases, it can happen 30 to 60 times per hour. This constant nocturnal "assault" leads to:
-
Oxidative Stress: The sudden re-introduction of oxygen after a pause creates free radicals that damage the lining of the blood vessels (endothelium).
-
Systemic Inflammation: Chronic low oxygen levels trigger inflammatory markers that accelerate the buildup of plaque in the arteries (atherosclerosis).
The Direct Route to High Blood Pressure
One of the most well-documented consequences of untreated sleep apnea is high blood pressure (hypertension). While many factors contribute to hypertension—diet, genetics, and exercise—sleep apnea is a primary driver of "resistant hypertension," or high blood pressure that does not respond well to medication.
During an apnea event, the sudden spikes in blood pressure aren't contained to the night. Over time, the body’s "set point" for blood pressure shifts. The nervous system becomes "overwired," maintaining a state of high tension even during the day.
Key Fact: Research suggests that up to 50% of people with hypertension also have obstructive sleep apnea. If you are struggling to control your numbers, the culprit might be your breathing while you sleep.
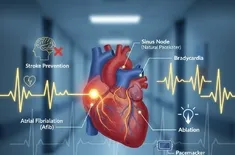
Atrial Fibrillation: The Electrical Disturbance
Beyond pressure, sleep apnea messes with the heart's electrical system. There is a significant correlation between sleep apnea and an atrial fibrillation cause. Atrial Fibrillation (AFib) is an irregular, often rapid heart rate that can lead to blood clots, stroke, and heart failure.
How does sleep apnea cause an arrhythmia?
-
Pressure Changes: When you try to inhale against a closed airway, it creates intense negative pressure in the chest. This physically stretches the walls of the heart’s upper chambers (the atria).
-
Electrical Remodeling: Over time, this stretching and the repeated cycles of low oxygen change the way electrical signals move through the heart, making it easier for AFib to take hold.
Patients with untreated sleep apnea are significantly more likely to see their AFib return even after successful medical procedures like cardioversion or ablation.
Recognizing the Red Flags
It is easy to dismiss the symptoms of sleep apnea as signs of aging or a busy lifestyle. However, recognizing these "hidden" markers can be life-saving.
The Warning Signs
-
Heavy Snoring: While not everyone who snores has apnea, chronic, loud snoring followed by silent pauses is a primary indicator.
-
Morning Headaches: Caused by the buildup of carbon dioxide in the blood overnight.
-
Excessive Daytime Sleepiness: Feeling like you could fall asleep at a red light or during a meeting.
-
Frequent Urination: Known as nocturia, this is often caused by the heart releasing a specific hormone (ANP) when it is stressed by apnea pressure changes.
Reversing the Risk: The Power of CPAP Benefits
The good news is that sleep apnea is highly treatable, and treating it can directly improve your heart health. The gold standard of treatment is Continuous Positive Airway Pressure (CPAP) therapy.
The CPAP benefits for the cardiovascular system are profound:
-
Stabilized Blood Pressure: Consistent use of CPAP has been shown to lower mean blood pressure, particularly the "dipping" at night that is crucial for heart health.
-
Reduced Arrhythmia Burden: For those with AFib, CPAP can reduce the frequency of episodes and improve the success rate of other heart treatments.
-
Endothelial Repair: Improved oxygenation allows the lining of your blood vessels to heal, reducing the risk of heart attack and stroke.
Long-Term Implications: A Path Forward
Ignoring the sleep apnea link to heart disease is a gamble with your longevity. If you or a loved one exhibits signs of disordered sleep, the first step is a diagnostic sleep study (polysomnography).
Modern technology has made this easier than ever, with many patients qualifying for home sleep tests. Once diagnosed, a combination of lifestyle changes—such as weight loss, avoiding alcohol before bed, and consistent device usage—can add years to your life and significantly reduce the strain on your cardiovascular system.
Summary of Cardiovascular Risks
| Condition | Sleep Apnea Connection |
| Hypertension | Sympathetic nervous system overactivity. |
| Heart Failure | Increased strain from negative chest pressure. |
| Stroke | Reduced blood flow and oxygen to the brain. |
| AFib | Structural and electrical changes to the atria. |