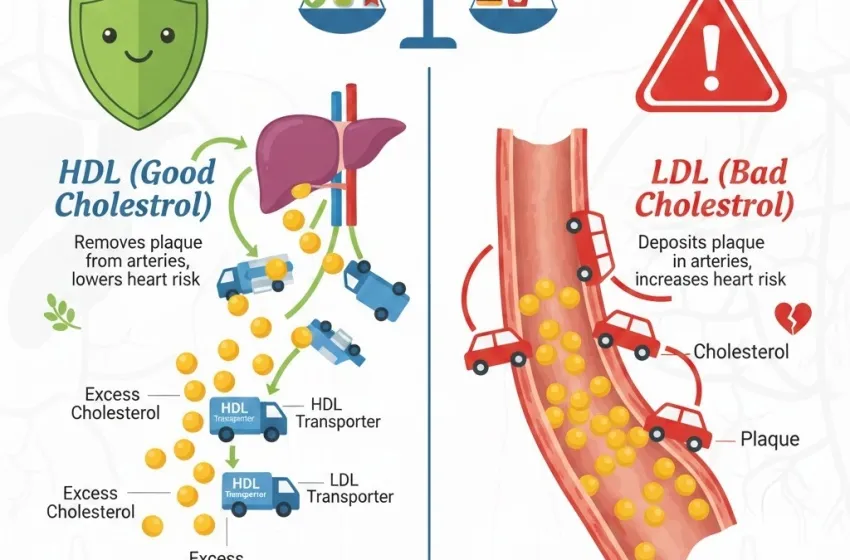
Understand the roles of HDL and LDL cholesterol
The terms "good cholesterol" and "bad cholesterol" are frequently used in health discussions, but what do they really mean for your body? Cholesterol is a waxy, fat-like substance found in every cell of your body. It's essential for creating cell membranes, producing hormones, and aiding in the digestion of fats. However, when cholesterol levels are imbalanced, it can pose significant risks to your cardiovascular health. The key players in this complex system are High-Density Lipoprotein (HDL) and Low-Density Lipoprotein (LDL). Understanding the distinct roles of these lipoproteins, the factors that influence their levels, and the necessary lifestyle changes is crucial for maintaining a healthy heart.
Differentiating the Roles of HDL and LDL
Cholesterol itself cannot travel through the bloodstream alone because it's a fat-like substance and blood is water-based. It must be packaged with proteins—forming lipoproteins. These packages act as transporters, moving cholesterol throughout the body.
High-Density Lipoprotein (HDL): The 'Good' Cholesterol
HDL is often dubbed the "good cholesterol" because of its protective role. Its primary function is called reverse cholesterol transport. Think of HDL as the scavenger or recycling truck of the circulatory system.
Role and Function:
HDL travels through the bloodstream, picking up excess cholesterol from cells and the walls of the arteries and transporting it back to the liver for removal or reprocessing. This action helps prevent the build-up of plaque.
Significance:
Higher HDL benefits are directly linked to a lower risk of heart disease and stroke. It is protective because it actively clears cholesterol from the arteries, preventing the first step in the process of atherosclerosis (arterial hardening).
Low-Density Lipoprotein (LDL): The 'Bad' Cholesterol
LDL is labeled the "bad cholesterol" because high levels are associated with increased cardiovascular danger.
Role and Function:
LDL's job is to carry cholesterol from the liver to the body’s cells, which need it for various functions. However, when there is too much LDL, the excess particles can begin to accumulate.
Significance:
The LDL risk is that when levels are too high, LDL particles can penetrate the lining of the artery walls. Once inside, they become oxidized and contribute to the formation of hard, fatty deposits known as plaque. This process narrows the arteries, restricting blood flow and leading to conditions like coronary artery disease, heart attack, and stroke.
The Role of Triglycerides
While HDL and LDL are the primary focus of cholesterol discussions, another type of fat in the blood, triglycerides, is also a vital component of a standard lipid panel.
Definition:
Triglycerides are the most common type of fat in the body. They store unused calories and provide energy.
Significance:
High levels of triglycerides, especially when combined with high LDL and low HDL, significantly increase the risk of heart disease. Elevated triglycerides are often a sign of high simple carbohydrate intake, excessive alcohol consumption, and lack of physical activity.
Determining Optimal Cholesterol Levels
A lipid panel is a blood test that measures your total cholesterol, LDL, HDL, and triglycerides. Interpreting these results helps determine your optimal cholesterol levels and overall cardiovascular risk. These are general guidelines, but your ideal targets may vary based on your personal health history, pre-existing conditions (like diabetes), and family history.
| Measurement | Optimal/Target Range (mg/dL) | Notes |
|---|---|---|
| Total Cholesterol | Less than 200 | Borderline High: 200–239, High: 240 and above |
| LDL Cholesterol | Less than 100 | Target for high-risk individuals (e.g., those with heart disease): Less than 70 |
| HDL Cholesterol | 60 or higher | Lower numbers are considered a risk factor |
| Triglycerides | Less than 150 | Borderline High: 150–199, High: 200–499 |
Aiming for a high HDL and a low LDL is the primary goal for heart health.
Dietary Strategies for Cholesterol Management
Diet is perhaps the most powerful tool for influencing your cholesterol profile. Simple, intentional changes can significantly impact your lipoprotein balance.
Actively Raising HDL (Good Cholesterol)
Since HDL is protective, raising its levels is an excellent strategy for heart health.
- Prioritize Monounsaturated Fats: Consuming healthy fats like olive oil (especially extra virgin) and avocado oil is linked to increased HDL levels.
- Increase Physical Activity: Regular, vigorous aerobic exercise (such as running, swimming, or brisk walking) is one of the most effective ways to raise HDL cholesterol. Aim for at least 150 minutes of moderate-intensity activity per week.
- Moderate Alcohol Consumption: While not a recommendation to start drinking, moderate intake (one drink per day for women, one to two for men) has been associated with higher HDL. However, the risks often outweigh this benefit, and this strategy should be discussed with a doctor.
- Quit Smoking: Smoking dramatically lowers HDL levels. Quitting smoking often leads to a significant and rapid rise in HDL.
- Incorporate Nuts and Seeds: Almonds, walnuts, and chia seeds provide healthy unsaturated fats and fiber, supporting HDL production.
Actively Lowering LDL (Bad Cholesterol)
The most effective strategy for reducing LDL involves modifying the type of dietary fat types you consume and increasing soluble fiber.
- Avoid Saturated and Trans Fats: This is the cornerstone of lowering LDL. Saturated fats are predominantly found in red meat, high-fat dairy products (butter, cheese, whole milk), and coconut and palm oils. Trans fats (partially hydrogenated oils) are often found in fried foods, commercial baked goods, and some margarines and should be eliminated entirely from the diet as they both raise LDL and lower HDL.
- Increase Soluble Fiber Intake: Soluble fiber binds to cholesterol in the digestive system, preventing its absorption and leading to its excretion. Excellent sources include:
- Oats and oat bran
- Barley
- Legumes (beans, lentils)
- Fruits (apples, citrus fruits, grapes, strawberries)
- Embrace Monounsaturated and Polyunsaturated Fats: Replacing saturated fats with healthy fats like those found in canola oil, sunflower oil, and fatty fish can actively lower LDL.
- Plant Sterols and Stanols: These naturally occurring compounds found in fortified foods (like some margarines and orange juices) can block the absorption of cholesterol in the small intestine, leading to a significant drop in LDL.
- Soy Products: Foods like tofu and edamame contain protein that may help lower LDL levels.
The Power of Omega-3 Fatty Acids
Omega-3 fatty acids are a type of polyunsaturated fat that plays a special and critical role in cardiovascular health. They are considered essential fats because the body cannot produce them and must obtain them through diet.
Impact on Lipids:
Omega-3s, particularly EPA and DHA found in fatty fish, are most renowned for their powerful ability to lower triglycerides. They also possess mild LDL-lowering and anti-inflammatory properties.
Sources:
The best sources are fatty cold-water fish (salmon, mackerel, herring, sardines, tuna). Plant-based sources (alpha-linolenic acid or ALA) include flaxseeds, chia seeds, and walnuts.
Beyond Diet: Lifestyle and Genetic Factors
While diet and exercise are primary levers for managing cholesterol, other factors also contribute to your lipid profile:
- Genetics: Some people have a genetic predisposition (like Familial Hypercholesterolemia) that causes very high LDL levels despite a perfect diet. For these individuals, medication (statins) is often necessary.
- Body Weight: Losing even a small amount of weight (5–10% of body weight) can significantly improve the lipid profile, including lowering LDL, total cholesterol, and triglycerides, and raising HDL.
- Smoking: As mentioned, smoking is detrimental, lowering HDL and promoting the oxidation of LDL, making it more dangerous.
- Medication: For individuals whose LDL levels remain dangerously high despite aggressive lifestyle changes, doctors may prescribe cholesterol-lowering medications like statins, which work by inhibiting the liver's production of cholesterol.
Conclusion
Managing cholesterol is a balancing act. It is not about eliminating cholesterol entirely, but about tilting the balance in favor of the protective HDL benefits and away from the elevated LDL risk. This is achieved through a multi-faceted approach centered on diet, physical activity, and awareness of genetic predispositions. By focusing on incorporating healthy fats like omega-3 and monounsaturated fats (like olive oil), reducing saturated and trans fats, increasing fiber intake, and getting regular exercise, you can actively work toward achieving optimal cholesterol levels and dramatically lowering your risk of cardiovascular disease. Regularly monitoring your triglycerides and other components of your lipid panel with your healthcare provider will ensure your strategy remains effective.