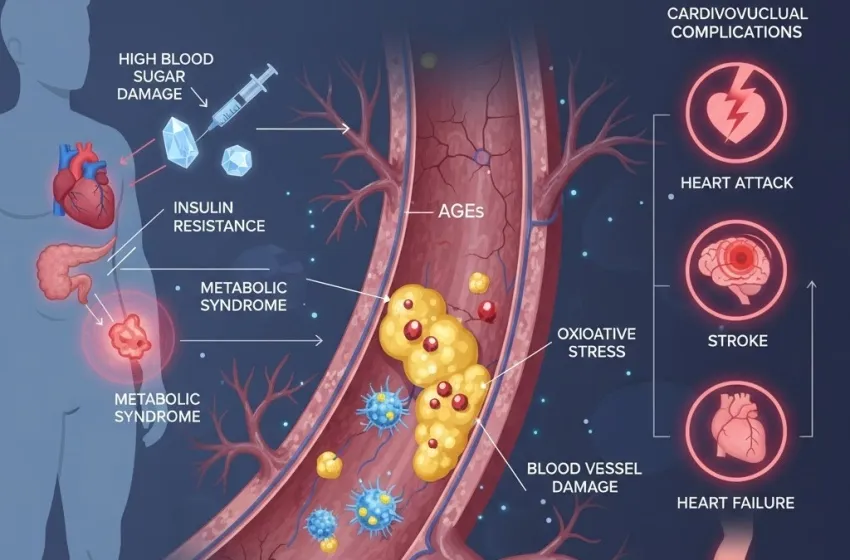
Learn how high blood sugar and insulin resistance cause blood vessel damage, making it a major, independent heart risk.
Diabetes mellitus is a global health crisis, affecting hundreds of millions of people. While managing high blood sugar is the most apparent daily challenge, the long-term, systemic consequences of this condition are far more devastating, particularly for the cardiovascular system. The link between diabetes and heart disease is not merely correlational; diabetes is a major, independent risk factor for a variety of heart conditions, significantly accelerating the process of atherosclerosis and dramatically increasing the risk of heart attacks, strokes, and heart failure.
This pervasive impact is why the risk of death from heart disease or stroke is about two to four times higher in people with diabetes. Understanding the underlying mechanisms—the chronic damage wrought by elevated glucose levels on the delicate blood vessel damage—is crucial for effective management and prevention.
Diabetes as an Independent Cardiovascular Threat
Why is diabetes considered an independent risk factor? It’s because the presence of diabetes, regardless of other traditional risk factors like high blood pressure, high cholesterol, smoking, or obesity, is enough to dramatically elevate diabetic heart risk. The chronic metabolic derangement inherent in diabetes acts as a continuous, systemic assault on the entire vascular network, making the development of cardiovascular complications almost inevitable without strict control.
This elevation of risk is partly explained by the fact that diabetes rarely occurs in isolation. It is frequently part of a cluster of conditions known as metabolic syndrome, which includes abdominal obesity, high blood pressure, and dyslipidemia (abnormal cholesterol/triglyceride levels). These conditions synergize to create a highly toxic environment for the heart and arteries. However, even when adjusting for these co-morbidities, the damage caused directly by hyperglycemia solidifies diabetes's role as a standalone threat.
The Mechanisms of Vascular Damage: How High Blood Sugar Kills Arteries
The long-term exposure to elevated glucose—the characteristic feature of uncontrolled diabetes—is the primary engine driving the accelerated development of heart disease. This damage occurs through several interconnected biochemical pathways, all centered on injuring the endothelium, the single-cell layer lining the inside of all blood vessel damage throughout the body.
Glycation and Advanced Glycation End Products (AGEs)
One of the most destructive processes is glycation. This is the non-enzymatic reaction between sugar molecules (like glucose) and proteins or lipids. Over time, these reactions form stable, harmful compounds called Advanced Glycation End Products (AGEs).
- Protein Cross-Linking: AGEs accumulate in the walls of blood vessels. They cause collagen, a main structural protein in the arterial wall, to become stiff, brittle, and less elastic. This process is a key contributor to arterial stiffness, a hallmark of advanced vascular disease.
- Endothelial Dysfunction: AGEs bind to specific receptors (RAGE) on endothelial cells, triggering chronic inflammation and oxidative stress. This severely impairs the normal function of the endothelium, specifically its ability to produce nitric oxide (NO), a critical molecule that signals the smooth muscle cells to relax and the vessel to dilate. When NO production is impaired, vessels struggle to open up, leading to hypertension and reduced blood flow.
Oxidative Stress: The Rusting of the Arteries
High blood sugar damage significantly increases the production of Reactive Oxygen Species (ROS), often referred to as free radicals, within the cells of the vascular wall.
- Mitochondrial Overload: Hyperglycemia overwhelms the mitochondria (the cell's powerhouses), leading to an overproduction of ROS.
- Cellular Injury: This oxidative stress is essentially "molecular rust" that damages proteins, lipids, and DNA within the vascular cells. It promotes the oxidation of LDL cholesterol (the "bad" cholesterol), making it far more easily taken up by macrophages to form foam cells—the initial building blocks of the atherosclerotic plaque.
The Polyol Pathway and PKC Activation
Two other major metabolic pathways, the polyol pathway and the activation of Protein Kinase C (PKC), are also activated by chronic hyperglycemia and contribute to the vascular injury. Both pathways disrupt cellular signaling, promote inflammation, and contribute to impaired blood flow and vessel leakage, especially in the microvasculature.
The Central Role of Insulin Resistance
The majority of people with type 2 diabetes also have insulin resistance, a condition where cells do not respond effectively to insulin. This is a critical driver of metabolic syndrome and heart disease, even before the onset of overt diabetes.
- Hyperinsulinemia: To overcome this resistance, the pancreas produces excessive amounts of insulin, a state called hyperinsulinemia. Insulin, in high concentrations, can act as a growth factor, promoting the proliferation of smooth muscle cells in the arterial wall. This contributes to the thickening and narrowing of the arteries.
- Dyslipidemia: Insulin resistance is closely linked to a characteristic pattern of abnormal blood fats (diabetic dyslipidemia): high triglycerides, low HDL (the "good" cholesterol), and the presence of small, dense, highly atherogenic LDL particles. This profile is profoundly harmful and significantly contributes to diabetic heart risk.
- Inflammation: Adipose (fat) tissue, particularly visceral fat associated with insulin resistance, releases pro-inflammatory cytokines, creating a state of chronic, low-grade systemic inflammation. This inflammation is a crucial trigger and perpetuator of atherosclerosis—the hardening and narrowing of the arteries.
The Spectrum of Cardiovascular Complications
The damage to the blood vessels, resulting from the cumulative effect of high blood sugar damage and insulin resistance, manifests in several severe cardiovascular complications:
Coronary Artery Disease (CAD)
This is the most common diabetic heart risk. Diabetes accelerates atherosclerosis in the coronary arteries (the vessels supplying the heart muscle). Plaque builds up faster, is more widespread, and is more prone to rupture, leading to a complete blockage and a Myocardial Infarction (Heart Attack). People with diabetes often experience "silent" heart attacks, where nerve damage (diabetic neuropathy) prevents them from feeling the typical chest pain (angina), delaying treatment and worsening the prognosis.
Stroke
The same atherosclerotic process that affects the coronary arteries impacts the carotid and cerebral arteries, increasing the risk of both Ischemic Stroke (due to a blockage) and Hemorrhagic Stroke (due to vessel rupture, though less common).
Heart Failure
Diabetes is a leading cause of Heart Failure (HF), often developing even without a prior history of a heart attack. This is due to a condition called Diabetic Cardiomyopathy.
- Diabetic Cardiomyopathy: This is structural and functional damage to the heart muscle itself, caused by prolonged metabolic syndrome and high glucose exposure. It leads to the stiffening and scarring (fibrosis) of the heart muscle, impairing its ability to pump blood effectively (systolic failure) or to relax and fill properly (diastolic failure).
Peripheral Artery Disease (PAD)
PAD involves the narrowing of arteries, typically in the legs and feet. This dramatically reduces blood flow, causing pain, non-healing ulcers, and ultimately, a high risk of amputation. This is a clear example of how chronic blood vessel damage specifically targets the micro and macrovasculature of the extremities.
Mitigation and Management: Breaking the Link
The profound diabetic heart risk underscores the critical importance of a multi-faceted management strategy. Simply focusing on A1C (average blood sugar) is insufficient; comprehensive management of the metabolic syndrome is essential to minimize cardiovascular complications.
- Glycemic Control (Targeting A1C): Tight control of blood glucose levels is paramount to preventing high blood sugar damage and the formation of AGEs. This is the foundation of preventing chronic vascular damage.
- Blood Pressure Control: Hypertension is a major accelerator of atherosclerosis. Aggressive management is necessary, as high blood pressure acts synergistically with diabetes to damage the endothelium.
- Lipid Management: Targeting the diabetic dyslipidemia—lowering LDL and triglycerides, and raising HDL—is critical. Statins are often prescribed to reduce overall diabetic heart risk.
- Lifestyle Modifications:
- Diet: A heart-healthy diet low in saturated fats, trans fats, and added sugars.
- Exercise: Regular physical activity improves insulin resistance, aids in weight loss, and directly benefits the vascular system by improving nitric oxide production.
- Weight Management: Reducing excess body fat, especially visceral fat, directly addresses insulin resistance and components of the metabolic syndrome.
- Modern Medications: Newer classes of diabetes medications (SGLT2 inhibitors and GLP-1 receptor agonists) have been shown to provide significant, independent cardiovascular benefits, reducing the risk of heart attack, stroke, and heart failure, demonstrating their power in mitigating the long-term blood vessel damage caused by diabetes.
Conclusion: A Preventable Burden
The fact that diabetes acts as a major independent risk factor for heart disease emphasizes the urgent need for early diagnosis and aggressive management. The systemic damage begins silently, with high blood sugar damage initiating a cascade of events—glycation, oxidative stress, and inflammation—that cripples the vascular system. Insulin resistance amplifies this damage, leading to a toxic lipid profile and accelerating the relentless march of atherosclerosis.
By recognizing the gravity of the diabetic heart risk and adopting a holistic strategy that targets not just glucose but also blood pressure, cholesterol, and lifestyle factors, it is possible to profoundly disrupt this critical link, reduce cardiovascular complications, and safeguard the long-term health and well-being of individuals living with diabetes.